Hours after giving birth, with her son rushed away to a high dependency unit, as she lay broken and bleeding, Morgan Joines overheard a midwife blaming her.
Her son had been born with wet lung after an emergency and traumatic caesarean section.
“I overheard [the midwife] tell a student nurse I was the reason my son was ill, because I was too lazy to push,” she told Sky News.
“I was broken. I genuinely believed for ages afterwards that I had failed my son.
“I thought I was the reason he was ill.”
Her son was born at John Radcliffe Hospital in Oxford, part of the Oxford University’s Hospital Trust. Morgan is one of more than 500 families who say they have been harmed by maternity care at the Trust.
On Monday, the health secretary, Wes Streeting, announced a “rapid” national investigation into NHS maternity services.
A taskforce, chaired by Mr Streeting and made up of experts and bereaved families, will first investigate up to ten of the most concerning maternity and neonatal units.
And campaigners – calling themselves the Families Failed by OUH Maternity Services – are calling for Oxford to be on that initial list.
‘I thought I was going to die’
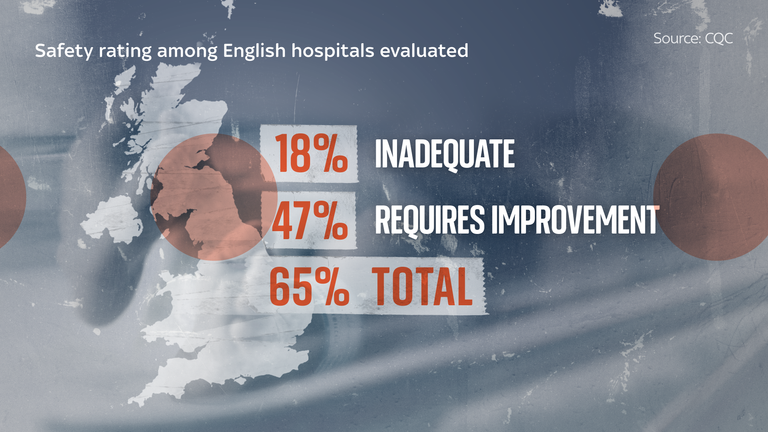
The unit was rated “requires improvement” in its last inspection by the government’s watchdog, the Care Quality Commission, in April 2023.
The CQC flagged issues around maintaining patient dignity, and said medicines were not always safely stored and managed. The unit did not manage the control of infection consistently it said, and wards were not always kept clean.
One mum told the campaign group she thought she was going to die after being left alone while in labour and denied pain relief.
Another said she is reluctant to consider having another child and feels a “profound loss of trust in the NHS”.
Trust to meet campaign group
Yvonne Christley, Chief Nursing Officer at OUH, said she apologised “for not being able to respond in detail about individual patient cases”.
“We regret any instance where we fail to provide the service that women and their families should expect. When this happens, we make every effort to review individual cases to understand what went wrong and how we can improve.”
She said the trust “make every effort” to keep women and families informed of what action it has taken, and said it is committed to maintaining an open dialogue with community groups.
“The Trust has agreed to meet with the campaign group and is eager to collaborate with them to implement the necessary changes and restore confidence in our services. These meetings are currently being scheduled.”
Caesarean sections account for approximately 40% of all births at OUH.
A ‘degrading strip wash’
A few hours after Morgan’s son had been whisked away to another part of the hospital, a nurse tried to force her to take oramorph, a high strength painkiller, she said.
When she declined to take the drug, having previously had a bad reaction, she said staff “claimed I was being difficult”.
“[They said] to just take the meds and get it over and done with.”
When Morgan was unable to get out of bed, she says the same nurse then gave her a “degrading” strip wash, without her consent.
The unit, she said, felt like it was against C-sections.
“Even though it was recommended by doctors that I had caesarean, it was medically necessary, I felt I should have done more to help him,” Morgan said.
Waiting eight hours for a C-section
When Kate* was 38 weeks pregnant with her third IVF baby, she was induced.
The doctors had tried to burst her waters, but realised her daughter was breech when the midwife felt her feet near the bottom of the birth canal, telling her: “I’m glad those didn’t break, I think I just felt a foot.”
At 11pm Kate reluctantly agreed to a C-section, but was told it was “safer to wait until the light of day” to go down to theatre.
She was sent away to an observation area experiencing intense contractions for more than six hours. In those hours, she said she was abandoned without pain relief and was bleeding.
“I felt so alone in the dead of night. My husband had been sent home, and I just wanted someone to talk to, someone to help me.
“I was in so much pain labouring but the midwife made me feel like a hypochondriac.”
She said the situation was escalating, she was becoming dehydrated, and her daughter’s heartrate was climbing, yet no one intervened.
A registrar who began his shift at 7am, examined her and rushed her immediately to theatre.
At this point she was 9cm dilated and the registrar was “shouting at me, telling me not to push.”
Kate’s daughter was her third IVF pregnancy, and she became emotional when she talked about what might have happened, had that registrar not examined her so quickly in the morning.
“They gambled with her life,” she said.
“If my waters had broken and that registrar wasn’t there, she would have started to come with her feet first. Both my boys had shot out, so I could be talking now as a mum who lost her child.
“It didn’t need to even get to that point.
“I should have had my C-section five hours earlier.”
After she had given birth, she was left “in a pool of my own blood, just covered in blood” and had to pull herself out of bed to clean up.
She said she joined the campaign in the hopes women will be listened to in the future and not have to endure what she did.
‘I can’t get my baby out’
Annika Weldon had three miscarriages before giving birth to her son.
“I remember lying on the ward, screaming in pain and none of the other ladies around me were screaming like I was,” she said.
“It didn’t feel right, obviously when you go into labour you expect you are going to be in pain, but I just knew there was something not right.”
The midwife who checked her when she was in active labour could not tell her if she was 1cm or 10cm dilated, she said.
“We spent 45 minutes trying to get my baby out but this midwife that I was with was just so uncaring, she didn’t really explain what I should be doing.”
She had said early in the pregnancy she told doctors she wanted a C-section and “was told I couldn’t have one”.
“I kind of accepted that unless it was an emergency situation, I wouldn’t be able to have one but then in that moment I was like, I don’t know what else I can do here. I feel completely exhausted; I can’t get my baby out.
“I was just so tired and exhausted.”
Her son was born not breathing and she was haemorrhaging blood.
She was taken to emergency surgery and the last thing she remembers before waking up in the ward is throwing up in her hair.
She wasn’t told until much later the extent of her blood loss (2.5L) when she was struggling to pick up her own baby: “When I asked for help, I was made to feel like an inconvenience.”
‘OUH is particularly bad’
For Kim Thomas, co-founder of Families Failed by OUH Maternity Services and CEO of the Birth Trauma Association, these stories are nothing new.
But Oxford University Hospitals Trust is “particularly bad”, she says.
“They seem to have this incredibly arrogant attitude. They won’t take criticism.
“Women who complain are routinely dismissed. There’s a failure to learn from mistakes.”
She says OUH also has “poor postnatal care”: “Dirty wards, blood on the floor, women left in their own blood, women not helped.”
Yvonne Christley, from OUH, said: “We are never complacent and welcome all feedback, whether positive or negative, as we learn from both.”
A Department of Health and Social Care spokesperson said: “Too many families have been devastated by serious failings in NHS maternity and neonatal care.
“They deserve swift answers, and urgent action is essential to prevent future tragedies.”
They said the government was “immensely grateful” to families for sharing their experiences.
“[We] will work closely with families on this journey to help ensure no parent or baby is ever let down again.”
The Oxford campaign group is growing daily, with more like Kate, Morgan and Annika joining the ranks of those calling for change.
And each day that passes without answers is a reminder of the trauma they endured.
“It still hurts to look back on. It’s taken a while for me to stop blaming myself, but it doesn’t get easier,” Morgan said.
*Some names have been changed.